Dermatitis is a common condition that affects millions of adults worldwide. It’s a broad term used to describe various skin conditions that cause inflammation, leading to symptoms like redness, itching, and irritation. Although dermatitis is not life-threatening, it can significantly affect a person’s quality of life due to the discomfort and the appearance of the skin. In this article, we will explore the different types of dermatitis in adults, the most common causes, and practical advice for prevention and management.
Definition of Dermatitis
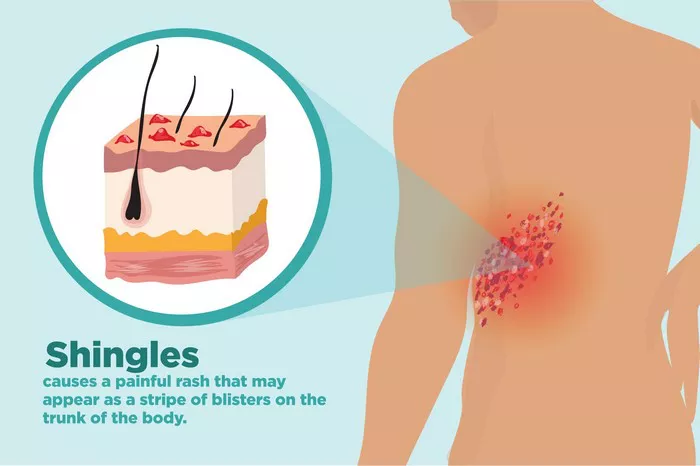
Dermatitis is an umbrella term for a group of skin conditions that result in inflammation. It is characterized by symptoms such as redness, swelling, itching, and, in some cases, blisters or sores. The condition can affect any part of the body but is most commonly found on the hands, face, and scalp.
SEE ALSO: How to Treat Vascular Dermatitis
Types of Dermatitis Commonly Found in Adults
Atopic Dermatitis: Often referred to as eczema, atopic dermatitis is a chronic condition that usually begins in childhood but can persist into adulthood. It is characterized by dry, itchy skin and is often associated with other allergic conditions like asthma and hay fever.
Contact Dermatitis: This type occurs when the skin comes into direct contact with an irritant or allergen. There are two main forms: irritant contact dermatitis, caused by exposure to irritating substances, and allergic contact dermatitis, triggered by an allergic reaction to a substance.
Seborrheic Dermatitis: This is a chronic form of dermatitis that primarily affects the scalp, but can also occur on other oily areas of the body like the face and chest. It’s characterized by red, scaly patches and dandruff.
Common Causes of Dermatitis in Adults
Understanding what causes dermatitis is crucial for effective management and prevention. The causes of dermatitis can be categorized into internal and external factors.
Internal Factors
Genetics:
One of the most significant internal factors in the development of dermatitis is genetics. A family history of dermatitis, eczema, asthma, or allergies can increase an individual’s likelihood of developing the condition. This genetic predisposition often manifests as an inherited tendency toward overactive immune responses, which can trigger inflammation in the skin.
Immune System:
The immune system plays a pivotal role in the development of dermatitis. In people with dermatitis, the immune system tends to be overactive, responding to even minor irritants or allergens with an inflammatory response. This response leads to the symptoms of dermatitis, such as redness, swelling, and itching. In autoimmune-related dermatitis, the immune system mistakenly attacks the skin, causing chronic inflammation and damage.
Underlying Medical Conditions:
Certain health conditions can increase the risk of developing dermatitis. For example:
Asthma and Allergies: People with asthma or other allergic conditions are more prone to atopic dermatitis due to the hyperactivity of their immune systems.
Hormonal Changes: Hormonal fluctuations, particularly during pregnancy or menopause, can trigger or exacerbate dermatitis.
Thyroid Disease: Conditions like hypothyroidism can contribute to skin dryness and susceptibility to dermatitis.
External Factors
Allergens:
Exposure to allergens is one of the most common external triggers of dermatitis. Substances like pollen, dust mites, pet dander, and certain foods can cause an allergic reaction, leading to contact dermatitis. Even products labeled as hypoallergenic can sometimes trigger a reaction in sensitive individuals.
Environmental Factors:
The environment plays a significant role in the development and exacerbation of dermatitis. Factors include:
Weather Conditions: Cold, dry air can lead to dry, cracked skin, increasing the risk of dermatitis. Conversely, hot and humid conditions can cause excessive sweating, which can also irritate the skin.
Pollution: Exposure to pollutants in the air can exacerbate skin inflammation, especially in those with pre-existing conditions like atopic dermatitis.
Water: Prolonged exposure to water, especially hard water, can strip the skin of natural oils, leading to dryness and irritation.
Practical Advice for Prevention
Preventing dermatitis involves managing both internal and external factors. Here are some strategies to help reduce the risk of developing dermatitis or managing it effectively if you already have it.
Identify and Avoid Triggers
The first step in preventing dermatitis is identifying and avoiding personal triggers. This can be done by keeping a diary of your symptoms and noting any potential triggers, such as specific foods, environmental factors, or stressful situations. Once identified, take steps to minimize exposure to these triggers. For example:
Keeping the skin well-hydrated is essential for preventing dermatitis. Here’s how:
Use Gentle Cleansers: Choose cleansers that are free of harsh chemicals, fragrances, and dyes. Opt for soap-free, pH-balanced products that won’t strip the skin of its natural oils.
Moisturize Regularly: Apply a moisturizer immediately after bathing to lock in moisture. Choose a thick, fragrance-free moisturizer that is suitable for your skin type. For extremely dry skin, you may want to use an ointment or cream instead of a lotion.
Avoid Hot Water: While a hot shower might feel good, it can dry out the skin and worsen dermatitis symptoms. Opt for lukewarm water instead, and limit your shower time to no more than 10-15 minutes.
Manage Stress
Since stress can exacerbate dermatitis, it’s important to find ways to manage it effectively. Consider the following stress-reducing techniques:
Exercise: Regular physical activity can help reduce stress and improve overall well-being. Activities like yoga, swimming, or even a daily walk can be beneficial.
Meditation and Mindfulness: Practicing mindfulness and meditation can help you manage stress more effectively. Techniques such as deep breathing, progressive muscle relaxation, and guided imagery can be particularly helpful.
Sleep: Ensure you’re getting enough sleep each night. Lack of sleep can weaken the immune system and increase stress levels, both of which can trigger or worsen dermatitis.
Conclusion
Dermatitis in adults is a complex condition with various causes, ranging from genetics and immune system factors to environmental triggers and stress. By understanding these causes and taking proactive steps to manage them, individuals can reduce their risk of developing dermatitis or manage existing symptoms more effectively. It’s crucial to identify and avoid personal triggers, maintain skin hydration, and manage stress levels. For those struggling with dermatitis, consulting a dermatologist and seeking support from relevant organizations can provide the necessary guidance and assistance. By following these strategies, you can improve your skin’s health and overall quality of life.
Related Topics: