Hidradenitis Suppurativa (HS) is a chronic skin condition characterized by the formation of painful, inflamed nodules, and abscesses, typically in areas where skin rubs together. While the physical toll on those affected is undeniable, understanding how Hidradenitis Suppurativa spreads is crucial for effective management and treatment of this challenging condition.
The Basics of Hidradenitis Suppurativa
Before delving into the spread of Hidradenitis Suppurativa, it is essential to grasp the basics of the condition. HS primarily affects areas with a high concentration of apocrine glands, such as the armpits, groin, buttocks, and under the breasts. These glands play a role in producing sweat and are often associated with hair follicles.
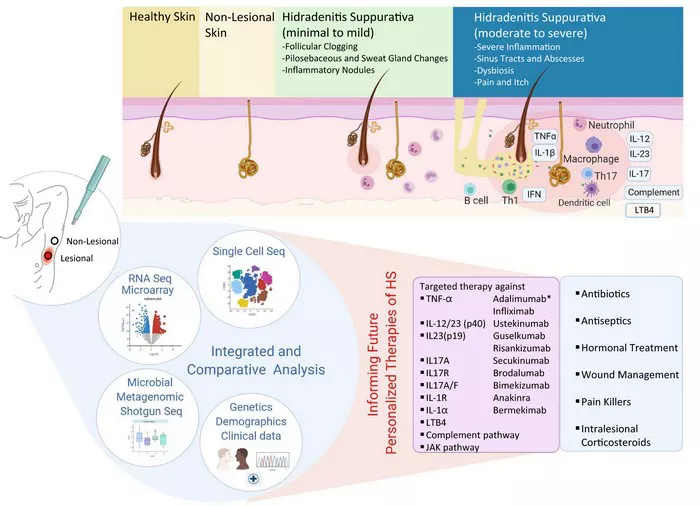
The hallmark of HS is the development of painful, recurrent nodules and abscesses, which can lead to the formation of sinus tracts or tunnels under the skin. The severity of symptoms can vary, with some individuals experiencing mild discomfort while others face debilitating pain and complications.
The Role of Genetics
Genetics is a significant factor in the development of Hidradenitis Suppurativa. Research indicates a strong familial predisposition, with individuals having a family history of HS being more likely to develop the condition themselves. Genetic factors contribute to the dysregulation of the immune system and the inflammation associated with HS.
The genetic component also sheds light on why HS tends to run in families. Specific genetic variations may increase the likelihood of an individual developing HS when exposed to certain triggers. While genetics alone do not determine the onset of HS, they play a crucial role in shaping an individual’s susceptibility to the condition.
Environmental Triggers and Lifestyle Factors
While genetics lay the groundwork, environmental triggers and lifestyle factors are equally instrumental in the spread and exacerbation of Hidradenitis Suppurativa. Obesity, smoking, and metabolic syndrome are known to be associated with an increased risk of HS. These factors contribute to systemic inflammation, further fueling the inflammatory processes seen in HS.
Poor personal hygiene and friction in skin folds are additional triggers that can aggravate the condition. Understanding these external factors is essential for individuals with HS, as modifying lifestyle and environmental elements can play a pivotal role in managing and preventing flare-ups.
The Microbiome Connection
Recent research has illuminated the role of the skin microbiome in the development and progression of Hidradenitis Suppurativa. The microbiome refers to the diverse community of microorganisms that inhabit the skin. In individuals with HS, there is evidence of dysbiosis, an imbalance in the normal microbial flora.
Changes in the microbiome can affect the skin’s barrier function, making it more susceptible to inflammation and infection. This altered microbial landscape may contribute to the formation of abscesses and nodules, further emphasizing the need to explore therapeutic interventions targeting the skin microbiome.
Contagion or Not?
One common misconception about Hidradenitis Suppurativa is whether it is contagious. It is crucial to dispel this myth and emphasize that HS is not a contagious condition. The spread of HS is not a result of direct person-to-person contact but rather a complex interplay of genetic, environmental, and microbial factors.
While HS itself is not contagious, the presence of certain risk factors within families or communities can contribute to a higher prevalence of the condition among closely related individuals. Education and awareness are key in dispelling misconceptions surrounding HS, promoting understanding, and reducing the stigma associated with the condition.
The Impact of Comorbidities
Hidradenitis Suppurativa rarely exists in isolation. Individuals with HS often experience a myriad of comorbidities, including but not limited to metabolic syndrome, inflammatory bowel disease, and autoimmune disorders. These comorbidities further complicate the clinical picture and may influence the spread of HS through shared underlying inflammatory pathways.
Understanding and addressing these associated conditions are integral to managing HS comprehensively. A multidisciplinary approach involving dermatologists, rheumatologists, and other specialists is often necessary to provide optimal care for individuals with Hidradenitis Suppurativa.
Advances in Treatment and Management
As our understanding of Hidradenitis Suppurativa deepens, so does the range of therapeutic options. While there is no cure for HS, various treatment modalities aim to alleviate symptoms, reduce inflammation, and prevent complications. Medical interventions, including antibiotics, anti-inflammatory medications, and biologics, are commonly employed to manage the condition.
Surgical interventions may be considered in severe cases, with procedures ranging from drainage of abscesses to more extensive excision of affected tissue. Lifestyle modifications, including weight management and smoking cessation, remain crucial components of a comprehensive treatment plan.
Conclusion
In conclusion, understanding how Hidradenitis Suppurativa spreads involves unraveling a complex web of genetic, environmental, and microbial factors. While genetics contribute to an individual’s susceptibility, environmental triggers and lifestyle factors play a significant role in the onset and exacerbation of the condition.
Dispelling myths about contagion, recognizing the impact of comorbidities, and embracing advances in treatment and management are essential steps in addressing Hidradenitis Suppurativa comprehensively. A holistic approach that considers the interplay of genetics, environment, and lifestyle factors is crucial for providing optimal care and improving the quality of life for those affected by this challenging skin condition.