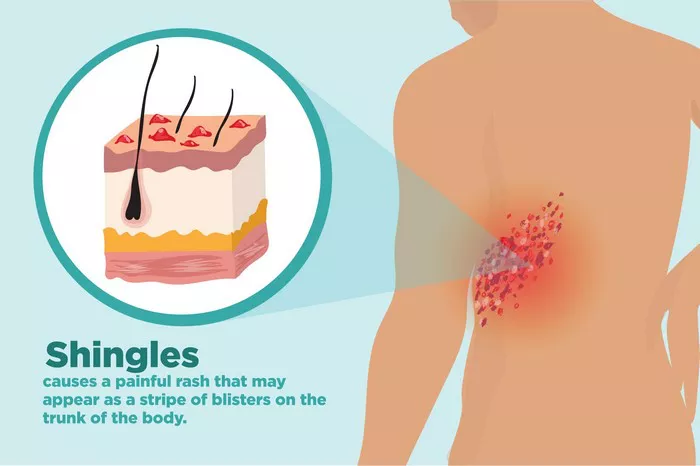
Eczema and vitiligo are both chronic skin conditions that affect millions of people worldwide. Despite their prevalence and the significant impact they can have on quality of life, these two disorders are fundamentally different in their pathophysiology, clinical presentation, and management. This article aims to explore whether there is any relationship between eczema and vitiligo, delving into their definitions, causes, symptoms, and treatments, and examining any potential connections between them.
Understanding Eczema
Definition and Types
Eczema, also known as atopic dermatitis, is a chronic inflammatory skin condition characterized by dry, itchy, and red skin. It is a common condition, particularly among children, though it can affect individuals of all ages. The term “eczema” can be broadly used to describe a group of conditions that cause the skin to become inflamed or irritated, including:
- Atopic Dermatitis: The most common form of eczema, often associated with other allergic conditions like asthma and hay fever.
- Contact Dermatitis: Caused by contact with irritants or allergens.
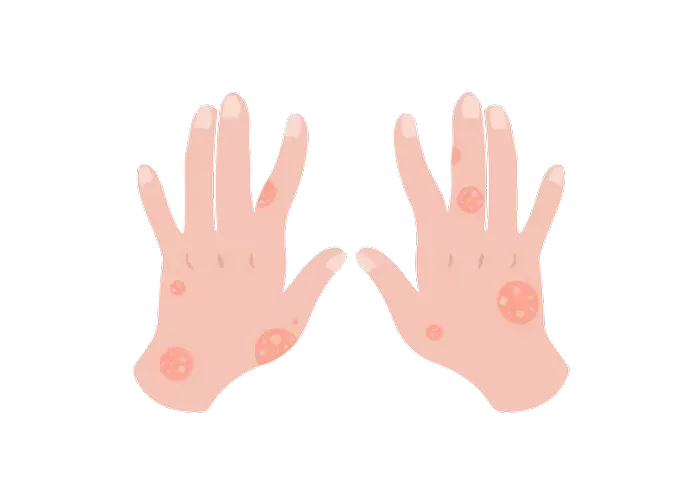
- Dyshidrotic Eczema: Affects the hands and feet, leading to itchy blisters.
- Nummular Eczema: Characterized by coin-shaped spots on the skin.
- Seborrheic Dermatitis: Often affects the scalp, causing scaly patches and dandruff.
- Stasis Dermatitis: Results from poor circulation in the lower legs.
Causes and Risk Factors
The exact cause of eczema is unknown, but it is believed to result from a combination of genetic and environmental factors. Key risk factors include:
- Genetics: A family history of eczema, asthma, or hay fever increases the likelihood of developing eczema.
- Immune System Dysfunction: An overactive immune response can trigger inflammation in the skin.
- Environmental Factors: Exposure to allergens (such as pollen, pet dander, and dust mites), irritants (such as soaps and detergents), and climate factors (such as cold weather or high humidity) can exacerbate eczema.
- Skin Barrier Defects: People with eczema often have a deficiency in certain proteins that maintain the skin barrier, making their skin more susceptible to irritants and allergens.
Symptoms and Diagnosis
The symptoms of eczema can vary widely but generally include:
- Itching: Often intense, leading to scratching and further skin damage.
- Redness and Inflammation: Affected areas of the skin become red and swollen.
- Dryness and Scaling: The skin may become dry, scaly, and cracked.
- Blisters: In some forms of eczema, small, fluid-filled blisters may develop.
Diagnosis typically involves a physical examination and a review of the patient’s medical history. In some cases, a skin biopsy or allergy testing may be performed to rule out other conditions or identify specific triggers.
Treatment and Management
There is no cure for eczema, but a variety of treatments can help manage symptoms and prevent flare-ups:
- Moisturizers: Regular use of emollients helps to maintain the skin barrier.
- Topical Steroids: These reduce inflammation and itching.
- Antihistamines: Oral medications can help control itching.
- Immunomodulators: Topical calcineurin inhibitors can be used as steroid-sparing agents.
- Lifestyle Changes: Identifying and avoiding triggers, maintaining a consistent skincare routine, and managing stress are crucial for controlling eczema.
Understanding Vitiligo
Definition and Types
Vitiligo is a long-term skin condition characterized by the loss of pigment, resulting in white patches on the skin. It occurs when melanocytes, the cells responsible for producing skin pigment, are destroyed. Vitiligo can be classified into several types based on the pattern and extent of depigmentation:
- Non-Segmental Vitiligo (NSV): The most common type, where white patches appear symmetrically on both sides of the body.
- Segmental Vitiligo (SV): Patches appear on one side of the body, often progressing rapidly within the first year and then stabilizing.
- Focal Vitiligo: Limited to one or a few areas without a clear segmental pattern.
- Universal Vitiligo: Involves more than 80% of the body surface.
Causes and Risk Factors
The exact cause of vitiligo is not fully understood, but several factors are believed to contribute to its development:
- Autoimmune Response: Vitiligo is often associated with an autoimmune reaction where the body’s immune system mistakenly attacks melanocytes.
- Genetics: A family history of vitiligo or other autoimmune diseases increases the risk.
- Environmental Triggers: Certain factors like sunburn, stress, or exposure to industrial chemicals may trigger or exacerbate vitiligo.
- Neurogenic Factors: Hypotheses suggest a link between vitiligo and the release of neurochemicals that affect melanocytes.
SEE ALSO: What Causes Vitiligo Later in Life
Symptoms and Diagnosis
Vitiligo’s primary symptom is the appearance of white patches on the skin, which may vary in size and location. Other symptoms can include:
- Premature Graying: Hair on the scalp, eyelashes, eyebrows, or beard may turn gray early.
- Change in Eye Color: The pigment of the retina may be affected.
- Loss of Pigment in Mucous Membranes: Inside the mouth or nose.
Diagnosis involves a clinical examination, medical history review, and sometimes a skin biopsy. Wood’s lamp (ultraviolet light) examination can help to identify depigmented areas more clearly.
Treatment and Management
While there is no cure for vitiligo, several treatments can help restore skin color or even out skin tone:
- Topical Corticosteroids: These may help to return pigment in some cases.
- Calcineurin Inhibitors: Topical medications that can be effective, especially for facial and neck areas.
- Phototherapy: UVB narrowband light therapy can stimulate melanocytes.
- Depigmentation: For extensive vitiligo, removing remaining pigment to achieve a uniform skin tone might be considered.
- Cosmetic Options: Makeup or self-tanners can help camouflage affected areas.
Exploring the Relationship Between Eczema and Vitiligo
Pathophysiological Differences
Eczema and vitiligo are fundamentally different in their underlying mechanisms:
- Eczema is primarily an inflammatory condition involving immune system hyperactivity and skin barrier dysfunction. It often occurs in individuals with a predisposition to allergic reactions.
- Vitiligo is primarily an autoimmune condition where the body’s immune system targets and destroys melanocytes, the pigment-producing cells in the skin.
- Despite these differences, there are areas of overlap that have intrigued researchers and clinicians.
Genetic and Immunological Overlaps
Recent studies suggest that there may be some genetic and immunological links between eczema and vitiligo:
- Shared Genetic Markers: Research has identified certain genetic markers that are associated with both eczema and vitiligo. For example, variants in genes involved in immune regulation and skin barrier function may predispose individuals to both conditions.
- Autoimmune Associations: Both conditions have been linked to autoimmune processes. Eczema is often seen in individuals with other autoimmune conditions, and vitiligo is frequently associated with autoimmune thyroid disease, rheumatoid arthritis, and type 1 diabetes.
Environmental Triggers and Immune System Interaction
Both eczema and vitiligo can be influenced by environmental factors and stress, suggesting that external triggers can play a significant role in their development and exacerbation:
- Environmental Triggers: Factors like stress, sun exposure, and skin trauma can exacerbate both conditions, indicating a complex interaction between external factors and the immune system.
- Immune System Dysregulation: In both conditions, there is evidence of immune system dysregulation, although the specific pathways and cells involved differ. Eczema involves a hyperactive immune response leading to inflammation, while vitiligo involves an autoimmune attack on melanocytes.
Clinical Co-Occurrence
While it is uncommon for eczema and vitiligo to co-occur, it is not impossible. When they do, it presents a unique challenge for diagnosis and treatment:
- Case Studies: There have been case reports of individuals with both eczema and vitiligo, suggesting a possible, though rare, coexistence.
- Diagnostic Challenges: The presence of one condition can sometimes mask the other, complicating diagnosis and management.
Implications for Treatment and Management
Understanding any potential relationship between eczema and vitiligo has important implications for treatment and management:
- Integrated Care: For individuals with both conditions, an integrated approach that addresses both the inflammatory and autoimmune aspects is crucial.
- Tailored Therapies: Recognizing the potential genetic and immunological overlaps may lead to more personalized treatment strategies that target the underlying mechanisms of both conditions.
- Patient Education: Educating patients about the nature of their conditions, potential triggers, and the importance of adhering to treatment regimens can improve outcomes.
Current Research and Future Directions
Ongoing research is crucial to further elucidate the relationship between eczema and vitiligo and to develop more effective treatments:
- Genetic Studies: Continued genetic research may identify more shared markers and pathways, offering new targets for therapy.
- Immunological Research: Understanding the immune mechanisms in greater detail could lead to new treatments that modulate the immune response more precisely.
- Clinical Trials: Well-designed clinical trials are needed to test new therapies and to better understand the effectiveness of existing treatments in patients with both conditions.
Conclusion
Eczema and vitiligo are distinct but potentially related skin conditions with significant implications for those affected. While they differ fundamentally in their pathophysiology, emerging research suggests that there may be genetic and immunological overlaps. Understanding these connections is crucial for developing more effective and integrated treatment strategies. As research continues, it is hoped that new insights will lead to improved outcomes for individuals living with these challenging conditions.
Related Topics: